Should I have genetic testing for Breast Cancer?
Inherited vs Non-inherited Cancer
Breast cancer is the most common female cancer affecting approximately 1 out of 8 women (~12%). The majority of breast cancer cases occur by chance, also referred to as sporadic.
We all carry certain genes (instruction codes) that are normally protective against cancer – they correct any DNA damage that naturally occurs when cells divide.
Inheriting faulty versions or “variants” of these genes – mutations, significantly raises your risk of developing cancer because the altered genes cannot repair the damaged cells which can build up and form a tumor (cancer).
Cancer is not usually inherited (in the family), but some types – mainly breast, ovarian, colorectal and prostate cancer – can be strongly influenced by genes and can run in families. Of diagnosed breast cancer cases, only 5-10% are hereditary; meaning they occur due to an inherited genetic change in the family.
Panel Testing
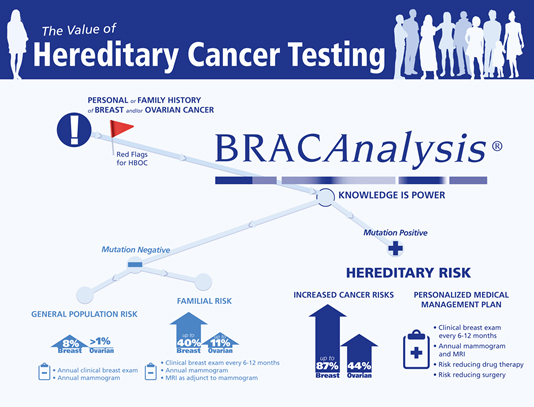
Multiple genes responsible for hereditary breast cancer have been discovered. Approximately 25% of hereditary breast cancer is due to mutations in one of two genes called BRCA1 and BRCA2. Another 20% of hereditary breast cancer is due to other known hereditary cancer genes. The application of ‘panel testing’ for breast cancer genetic testing is so far a matter of discussion. Standard practice still follows; in a first step, carrying out a BRCA 1 and 2 genetic test to identify any breast cancer causing mutations. However, if the woman tests negative, in a second step, she could then be offered a panel test of 21 (or more) breast cancer related genes to identify the disease causing mutation.
WHO SHOULD HAVE A GENETIC TEST?
- • Women with breast cancer diagnosed prior to menopause (or below the age of 50)
- • Women having three or more close relatives (mother, sisters, aunts) affected with breast cancer
- • Women who have cancer in both breasts
- • Women who have had ovarian cancer at any age
- • Women who have both Breast AND ovarian cancer
- • Women who have male breast cancer in the family
Advantages of testing:
- • Relief
- • Personalized medical recommendations
- • Risk reduction options – mastectomy (breast removal surgery), oophorectomy (removal of ovaries)
- • Results guide in developing management/screening program
- • Informative for other family members – can chose to have predictive testing
Disadvantages to testing for BRCA mutations:
- •Worry, Stress, Panic
- •Anxiety of sharing the information with the family (some of whom may also be at increased risk for breast cancer)
- •Women who test negative may falsely believe they will never get breast cancer
- •Complications with health insurance
What sort of results to expect?
Positive Result: A cancer-causing mutation is identified – risk for associated cancers is increased.
First-degree relatives, including parents, siblings, and children, have a 50% chance to carry the same mutation.
Genetic counseling is recommended for all family members to clarify their risks.
Negative Result: No breast cancer-causing mutation is detected in the genes included in the panel.
The significance of a negative result is dependent upon each individual’s personal family history. It is important to discuss the
significance of a negative result with your physician or genetic counselor.
Variant of Unclassified Significance: A genetic change referred to as a variant is identified in one of the genes in the cancer panel.
Variants, which are changes in the gene structure, may or may not have a harmful effect on how the gene functions.
The laboratory does not have enough information to determine if the variant results in an increased risk for cancer or not. Further research needs to be carried out to understand whether the change is harmful or not.
Should people considering genetic testing talk with a genetic counselor?
Genetic counseling is generally recommended before and after any genetic test for an inherited cancer syndrome. This counseling should be performed by a health care professional who is experienced in cancer genetics and counseling. Genetic counseling usually covers many aspects of the testing process, including:
- • A hereditary cancer risk assessment based on an individual’s personal and family medical history
- • Discussion of:
- • The appropriateness of genetic testing
- • The medical implications of a positive or a negative test result
- • The possibility that a test result might not be informative
- • The psychological risks and benefits of genetic test results
- • The risk of passing a mutation to children
- • Explanation of the specific test(s) that might be used and the technical accuracy of the test(s)

